Abstract

Introduction
Management of patients with hematologic malignancies (HM) post induction chemotherapy or allogeneic hematopoietic cell transplant (Allo HSCT) is often complicated by neutropenic fever associated with nodular pulmonary infiltrates, and may result in acute respiratory failure and death. The presence of a halo sign in a neutropenic patient with nodular infiltrates is highly suggestive of invasive pulmonary aspergillosis (IPA).
Fiberoptic bronchoscopy (FOB) with bronchoalveolar lavage (BAL) is the preferred procedure for identifying the infectious aetiology of pulmonary infiltrates in post Allo-HSCT or post chemotherapy in HM patients with neutropenic fever. The diagnostic value of FOB with BAL in such patients is controversial, however, it has been suggested that the microbiologic yield from FOB and BAL is higher when bronchoscopy is performed within 24 hours of presentation, allowing subsequent BAL-guided therapeutic adjustment.
With a view towards improving health care resource utilization, we re-evaluated this diagnostic strategy.
Methods
We conducted a prospective observational study of 100 participants with the following diagnoses: acute myeloid leukemia (AML), 76%; myelodysplastic syndrome (MDS), 9%; acute lymphoblastic leukemia (ALL), 6%; and acute promyelocytic leukemia (APL), 6%. One hundred sequential patients who underwent FOB after August 2016 and provided informed consent, were enrolled and followed for 30 days. Sixty six percent were admitted for induction chemotherapy; 17% for re-induction chemotherapy; 10% for conditioning pre- Allo- HSCT; 4% for consolidation chemotherapy; and 3% for other therapy.
Data collected included patients' demographics, dates of onset of fever and of baseline chest CT scan, findings on CT scan, dates of initiation of empirical antibiotic and antifungal therapy, BAL results, and the impact on antimicrobial choices. Other outcomes included transfer to ICU and death.
We assessed the utility of performing early FOB (within 48 hours of performing a low dose chest CT scan) vs Late FOB (after 48 hours from low dose chest CT scan) in post-chemotherapy HM and Allo-HSCT patients.
Results
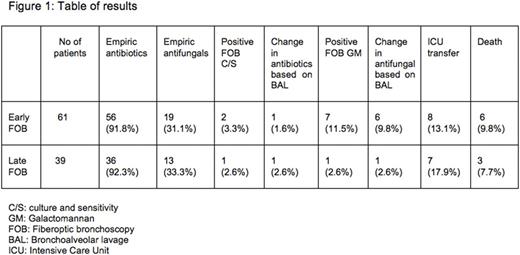
Of the 100 enrolled participants, 61 and 39 underwent early and late FOB, respectively (Figure-1: Table of results) . A positive BAL Galactomannan was observed in 7 (11.5%) early FOB cases, compared to only 1 (2.6 %) in late FOB case (p=0.15), with a subsequent impact on the choice of antifungal in 6 cases (9.8 %) and 1 case (2.6 %), respectively (p=0.042).
BAL culture was positive in 2 cases (3.3%) in the early FOB group, compared to only 1 case (2.6%) in the late FOB group (p=0.99). The choice of antibiotic was influenced by BAL results in 1 of the 2 early FOB cases.
Eight (13.3%) and 7 (17.9%) of early and late FOB patients, respectively, were transferred to the ICU (p=0.57); and 6 (9.8%) of the early FOB and 3 (7.7 %) of late FOB patients died (p=0.99).
Conclusion
The diagnostic yield of early FOB was greater than that of late FOB, as assessed by GM positivity, and more frequently permitted targeted antifungal therapy. There was no difference in the rate of antibiotic use between the two groups.
Gupta: Incyte: Consultancy, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Schuh: Amgen: Consultancy, Honoraria. Yee: Astex: Research Funding; Oncoethix: Research Funding; Karyopharm: Research Funding; Novartis Canada: Honoraria; Celgene Canada: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal